Vision & Reflex Clinic
Carrie Punger, OTD, OTR/L - Director
Vision and Reflex Clinic
Vision Rehabilitation
a. What is Vision Rehabilitation?
b. Vision Therapy or Occupational Therapy?
c. How Can Occupational Therapy Help?
Reflex Clinic
a. What are Primitive Reflexes?
c. How Can Occupational Therapy Help?








Vision Rehabilitation
a. What is Vision Rehabilitation?
Occupational therapists (OTs) provide vision rehabilitation by helping individuals improve their visual skills and use their remaining vision effectively for daily activities. They work on skills like visual attention, tracking, processing, and integration, aiming to enhance posture, body awareness, and movement coordination. OTs also focus on teaching adaptive strategies and using assistive technology to maximize independence.
Here's a more detailed look at how OTs approach vision rehab:
Comprehensive Evaluation:
OTs assess an individual's visual abilities and how current visual skills impact their daily life.
Functional Vision Exercises:
OTs may use exercises to improve visual skills like eye alignment, tracking, and visual processing.
Adaptive Equipment and Technology:
OTs can recommend and train individuals on using assistive devices and technologies to enhance visual function.
Environmental Modifications:
OTs can make recommendations for home/school modifications to optimize visual accessibility and safety.
Collaboration:
OTs often collaborate with other professionals like optometrists, ophthalmologists, and other therapists to develop comprehensive rehabilitation plans. Ultimately, patients benefit from this collaborative care approach. The goal of occupational therapy is to facilitate a patient’s ability to perform with the highest degree of independence possible. When the eye doctor is involved in the diagnosis and treatment of visual disorders, patients have access to the right vision care that addresses their individual needs.
Together, this team of professionals can help patients feel better, live safer, think more clearly, and enjoy engaging in meaningful life experiences.
b. Vision Therapy or Occupational Therapy?
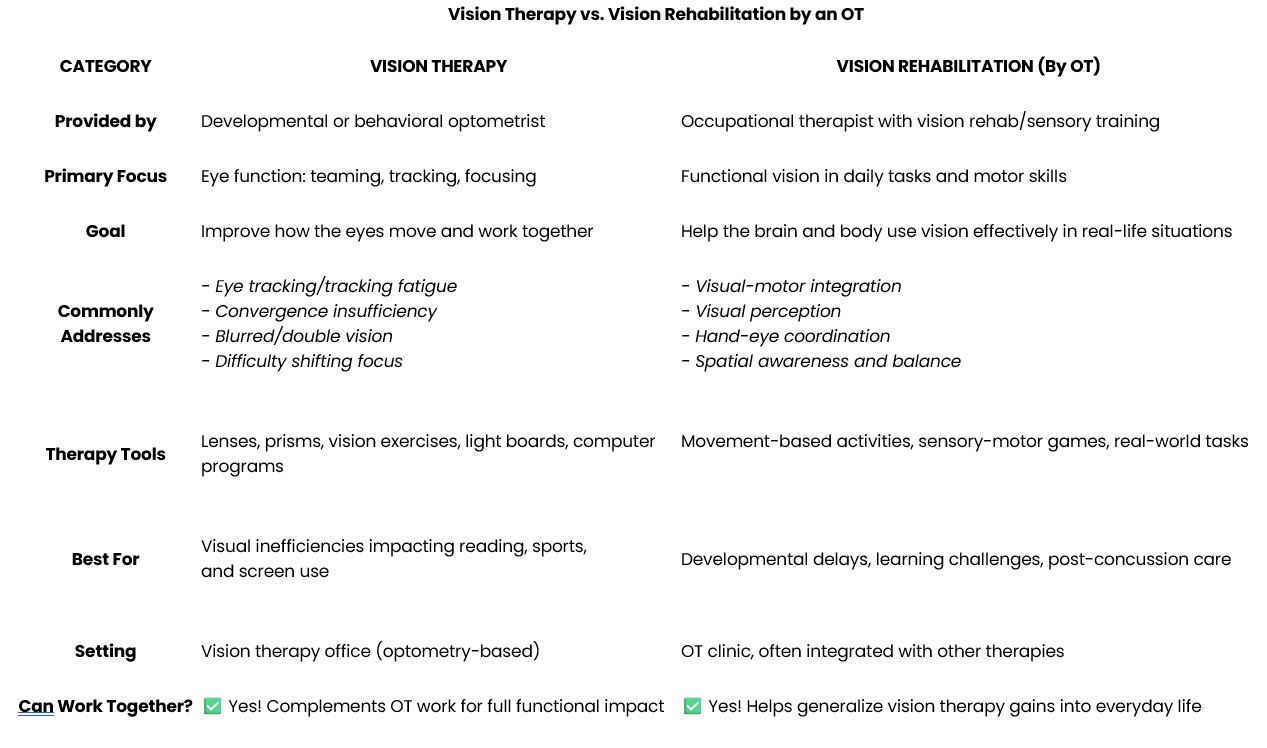
Vision Therapy vs. Vision Rehabilitation by an OT
When a child or adult struggles with visual skills, there are two different (but often complementary) approaches to help: vision therapy and vision rehabilitation by an occupational therapist (OT). While they may address some of the same challenges, they come from different backgrounds and serve slightly different purposes.
Vision Therapy
Provided by: Optometrists with specialized training in developmental or behavioral vision
Focus: Eye function and coordination
Goal: Improve the physical skills of the eyes—like tracking, teaming, focusing, and visual processing.
Commonly helps with:
Convergence insufficiency (eyes not working well together)
Double vision or blurred vision
Eye fatigue or headaches
Trouble shifting focus between near and far
Visual issues related to reading or screen use
Tools may include: Prism lenses, therapeutic filters, computer-based visual exercises, or in-office vision training tools.
Vision Rehabilitation by an Occupational Therapist (OT)
Provided by: Occupational therapists with training in functional vision and sensory integration
Focus: How vision impacts daily life, motor skills, and learning
Goal: Strengthen the use of vision in real-world tasks like writing, copying, balance, coordination, and spatial awareness.
Commonly helps with:
Visual-motor integration (hand-eye coordination)
Visual perceptual skills (understanding and interpreting what you see)
Navigating space, balance, and posture
Functional challenges after concussion or developmental delays
Incorporating vision into multisensory processing
Tools may include: Movement-based therapy, reflex integration, sensory-motor activities, games, and real-life tasks.
While vision therapy strengthens the eyes and their coordination, OT helps clients apply those skills in meaningful, functional ways throughout the day.
At Greater Atlanta Speech and Language Clinics’ Vision Clinic, we collaborate with optometrists and other specialists to create a comprehensive, individualized plan that meets your child's unique needs.
How can Occupational therapy help?
Primitive reflexes live in the brainstem, which is one of the most primitive parts of the brain. If reflexes do not integrate properly, it means the brainstem is still overly involved, and the cortex, which controls thinking, focus, planning, and emotion regulation, does not mature. Occupational therapists (OTs) employ a bottom-up approach, focusing on the body and nervous system first, building from the foundation to integrate primitive reflexes, enhance sensory processing, and improve postural control, which form the foundation for the development of higher-level skills. This bottom-up approach will incorporate a holistic treatment strategy to ensure functional outcomes that extend beyond integrating the reflexes.
Why Do Reflexes Matter?
When these reflexes don’t fully integrate, they can interfere with everyday functions such as:
Learning and attention
Emotional regulation
Coordination and balance
Visual tracking (important for reading)
Speech and language development
How Our Reflex Clinic Helps
Our Reflex Clinic identifies retained reflexes and uses gentle, movement-based activities to help the brain and body work together more efficiently. These exercises support:
Stronger motor skills
Better focus and behavior
Enhanced communication
Greater success in therapy and academics
Whether your child is experiencing developmental delays, ADHD, sensory issues, or learning differences, our team is here to provide a personalized plan to support lasting growth.
What are Primitive Reflexes?
Primitive reflexes are involuntary movement patterns initiated in the brainstem that help an infant survive and develop after birth. These reflexes elicit movements controlled by the brainstem that impact head righting, tone, and postural control, regardless of cortical brain development. Developmentally primitive reflexes appear in vitro and should be dormant by approximately 12 months of age. As a child develops typically, more mature postural reflexes emerge to aid in the development of necessary mature motor skills.
Why do they remain active?
The presence of primitive reflexes in children beyond the expected age of integration indicates immature central nervous system development. Delayed reflex integration may be due to a response to trauma at birth or after, too much time in seaters and swings, lack of tummy time, or c-section, etc. Additionally, these delays could be part of other disorders such as Attention Deficit Hyperactivity Disorder (ADHD), sensory processing disorder (SPD), autism, or learning disabilities (LD).
Primary Reflexes and Symptoms you might see:
Moro Reflex (Startle Reflex)
What to look for: Overreacts to sudden noises, light, or movement; may seem anxious, easily startled, or have poor balance and coordination.
Behavioral signs: Emotional sensitivity, fight-or-flight responses, anxiety, motion sickness.
ATNR (Asymmetrical Tonic Neck Reflex)
What to look for: When the head turns, one arm extends while the other bends (like a fencing pose).
Behavioral signs: Difficulty with handwriting, poor hand-eye coordination, and trouble crossing the midline (e.g., struggling to read across a page)
STNR (Symmetrical Tonic Neck Reflex)
What to look for: Head down = arms bend, legs straighten. Head up = arms straighten, legs bend.
Behavioral signs: Poor posture, w-sitting, difficulty sitting still or copying from a board, clumsiness.
TLR (Tonic Labyrinthine Reflex)
What to look for: When the head tilts back, the body stiffens, back arches.
Behavioral signs: Poor balance, motion sickness, slumped posture, trouble with activities requiring coordination.
Palmar Grasp Reflex
What to look for: Difficulty with fine motor skills, like writing or buttoning.
Behavioral signs: Pencil grip issues, hand fatigue, messy handwriting.
Other Symptoms You Might Notice:
Seems clumsy or uncoordinated.
Difficulty with focus or sitting still.
Emotional outbursts or sensitivity.
Trouble with reading, writing, or left-right confusion.
Poor posture or unusual sitting positions, such as w-sitting.
Issues with motor milestones (such as crawling, walking, and jumping)
Poor ocular motor skills
How Can an Occupational Therapist (OT) Help?
Helping the Brain and Eyes Work Together for Everyday Success
Occupational therapists (OTs) are trained to understand how vision affects daily function—not just how we see, but how we use what we see to move, learn, and interact with the world.
Here’s how OTs approach vision rehabilitation:
✅ 1. Assess Functional Vision Skills
OTs evaluate how visual challenges are impacting a child’s everyday activities, not just their ability to read an eye chart.
They look at:
Eye tracking (can the eyes follow moving objects smoothly?)
Eye teaming (do the eyes work together or drift apart?)
Visual perception (can the brain interpret what it sees?)
Hand-eye coordination (how well do the eyes and hands work together?)
Balance and spatial awareness (can the person navigate space safely?)
✅ 2. Identify Underlying Issues
Sometimes visual struggles are linked to:
Retained primitive reflexes
Sensory processing difficulties
Developmental delays
Brain injuries or concussions
OTs look at the whole person, identifying what’s holding back visual development.
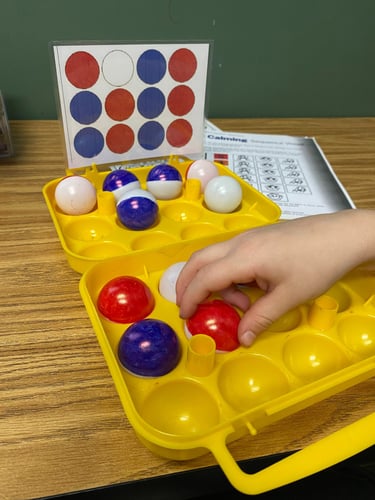
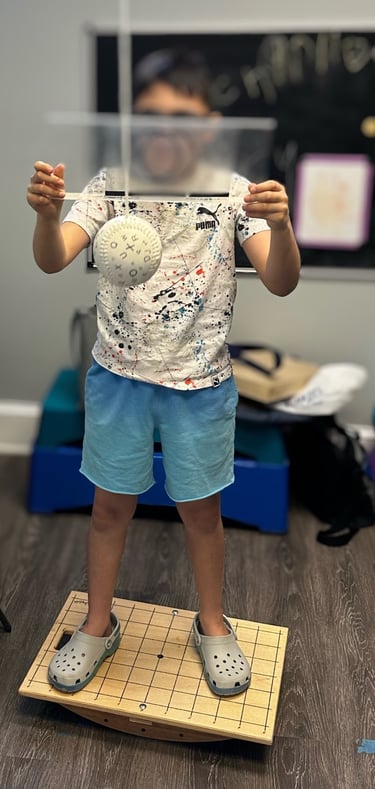
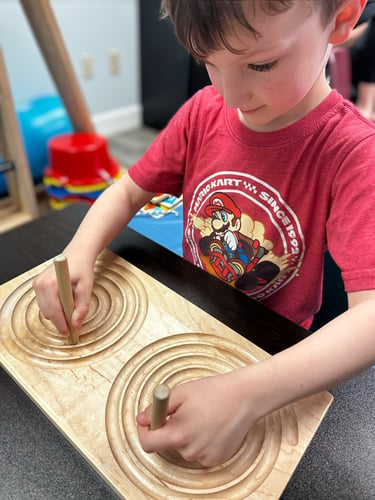
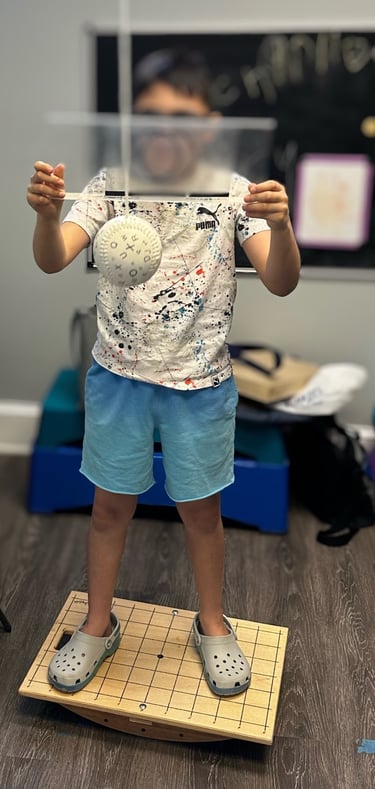
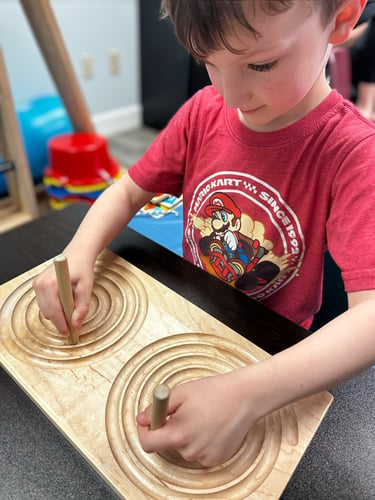
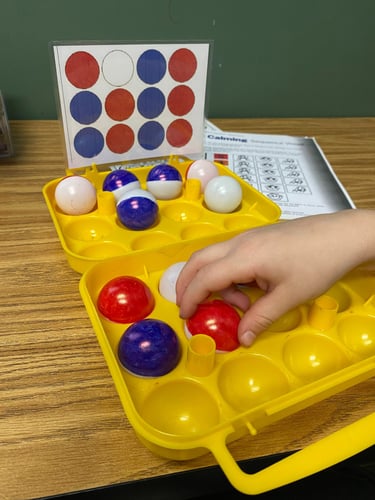
✅ 3. Use Movement-Based and Sensory Activities
Vision is deeply connected to movement and the nervous system, so therapy often looks like fun, play-based activities—but each one is purposeful!
Some examples:
Ball games to build tracking and depth perception
Obstacle courses to improve spatial awareness and coordination
Puzzles or mazes to develop visual discrimination
Swinging or balance boards to integrate vision with movement
Copying or drawing tasks to strengthen visual-motor skills
✅ 4. Reinforce Visual Skills in Real-Life Tasks
OTs help clients apply visual improvements to daily activities like:
Writing, reading, and copying from the board
Playing sports
Navigating hallways or classrooms
Getting dressed or brushing teeth
Organizing and planning tasks
✅ 5. Collaborate with Other Specialists
If a client also needs vision therapy (from an optometrist), OTs can coordinate care to maximize progress. It’s a team effort!
Contact Us


Main Clinic Building
1515 Johnson Ferry Road
Suite 100
Marietta, GA 30062
OT / PT Annex
1503 Johnson Ferry Road
Terrace Level
Marietta, GA 30062
Appointment Request: Click Here
Phone: (770) 977-9457
Fax: (770) 977-5087
Email: greateratlantaspeech@gmail.com
